The following was written by Hilary N. Karasz for Public Health Insider:
Sexually transmitted diseases (STDs) are on the rise across the U.S. and Washington and King County data show a similar trend towards more syphilis, gonorrhea, and chlamydia. Bottom line: We need to rein in what’s looking like an explosion of preventable, sexually transmitted disease. We need more surveillance to find STD cases, more awareness among healthcare providers, and more testing of people at risk. And depending on their risk status, sexually active people can create a safer sex plan about using condoms, having sex with fewer people, and testing more frequently.
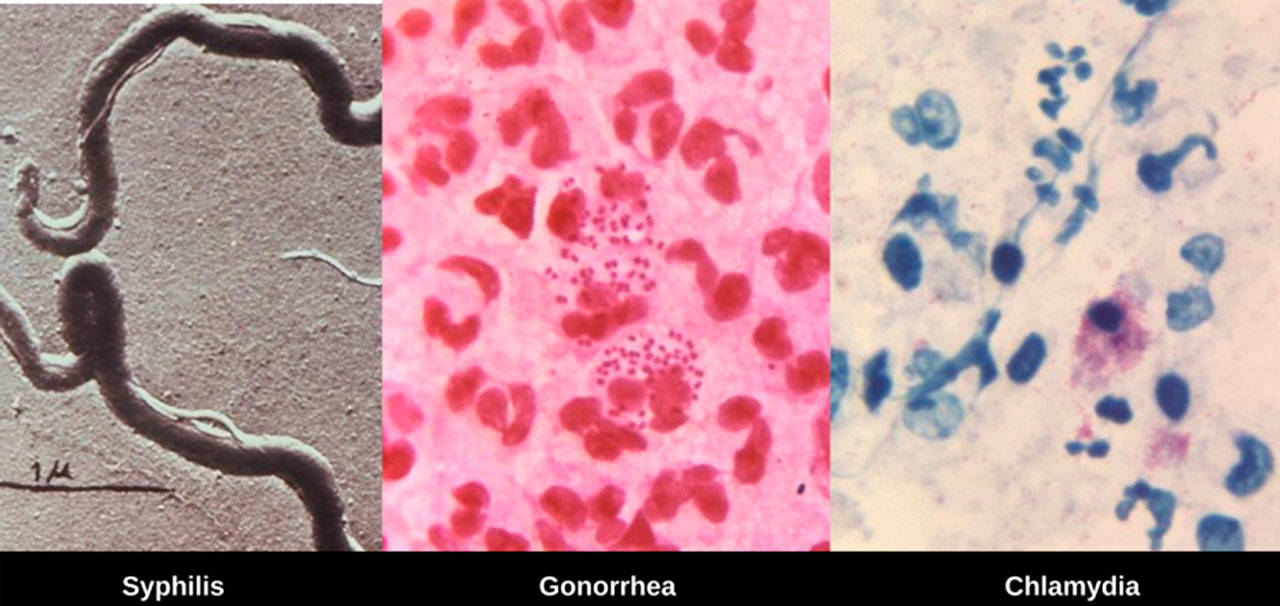
A tale of three STDs
Compared to 2015, King County data from 2016 show:
- Syphilis up 11% overall – with a doubling of cases among women and increases among men as well.
- Gonorrhea up 15% overall, primarily among men who have sex with men (MSM)
- Chlamydia up 11% — among MSM, women and heterosexual men.
This increase over the past year is consistent with an upward trend we reported on in the Public Health Insider in 2016.
Dr. Lindley Barbee, MD, MPH, of Public Health – Seattle & King County’s STD clinic told the Insider that increases in syphilis among women present a risk of transmission to unborn babies, a dangerous and completely preventable condition called congenital syphilis that causes severe health complications and death in infants. More than 600 cases of congenital syphilis were reported nation-wide in 2016. Locally, we were able to identify and treat women infected with syphilis prior to delivery, but 5 cases of congenital syphilis were reported in Washington State in 2016.
Dr. Barbee said that data show an increase of 15% of gonorrhea, primarily among MSM. This increase may be due in part to more accurate and complete testing of people who are at risk for the disease, but a good portion of the increase is due to true increases in disease transmission.
Young women are typically more likely to be diagnosed with chlamydia in the United States (due to screening recommendations for women under 25), but as is the case nationally, the disease is spreading among men as well in King County.
These three sexually transmitted diseases can be cured with antibiotics. Left untreated, they can cause infertility, ectopic pregnancies, still-birth, increased risk of HIV, both transmission and acquisition, and death, among other dangerous health outcomes.
The upward trend
While some of the increase in numbers may be due to increased testing, (i.e. we’re just getting better at finding cases) in fact, more people are coming down with these diseases. The question is why – and as with anything as complicated as STDs there are likely multiple causes. For example, among MSM, one key change is that as HIV is now preventable through anti-viral drugs (e.g. Pre-exposure prophylaxis or PrePand HIV medications). As a result, fewer people are using condoms and are engaging in more risky behaviors (e.g. having condomless receptive anal intercourse, having sex with anonymous partners, and having sex with multiple partners). Injection drug use may be playing a part in the increase in syphilis, particularly among people living homeless. And chlamydia? It’s likely both increased surveillance and a decrease in public health prevention resources.
What’s next in prevention
Protecting people from the spread of sexually transmitted disease is essential to keeping our communities healthy. With more disease, more people are exposed but with our limited resources our ability to conduct important activities such as partner notification and surveillance is strained. Public Health simply doesn’t have the resources to do everything we should to stop the spread of disease. We need more money and we need to get more creative.
For example, to prevent congenital syphilis high risk pregnant women need appropriate pre-natal care. Women who do not want to have a baby in the first place must have access to and use effective contraception such as such as IUDs. And because over the past decade or so, syphilis has been primarily a disease of MSM, we have to re-educate health care providers to think about syphilis screening when treating non-MSM patients. We may also have to expand our screening outside of traditional venues. We have already talked to ER doctors about screening heterosexuals who are homeless and/or drug-using. And, we may need to expand STD screening, especially syphilis screening, to new locations such as our needle exchange.
As long as humans have sex, STDs will present a risk. We can prevent the spread of disease with a better informed public using condoms appropriately and testing frequently when at higher risk, better informed health care providers on the lookout for these diseases in new populations, and a better resourced public health system to track and prevent outbreaks.