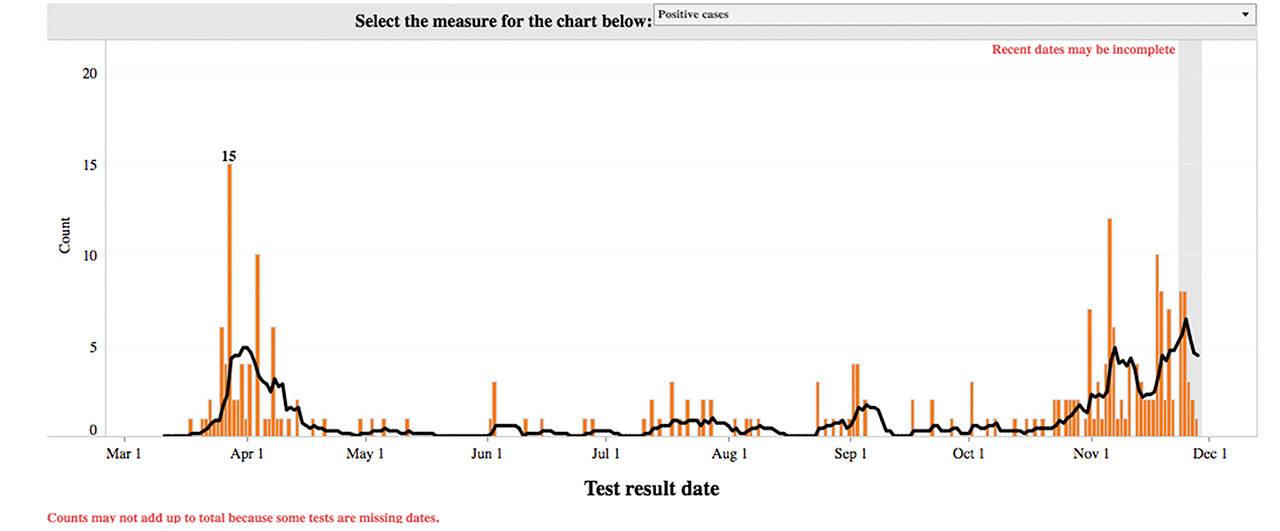
Enumclaw’s number of COVID-19 cases are ramping up.
October was a relatively quiet month after small spikes were seen in August and September; only about 22 cases of the coronavirus were reported, most of which happened at the end of the month.
But November quickly outpaced October’s numbers. As of Sunday, Nov. 29, the city suffered 106 additional cases that month, bringing Enumclaw’s total COVID-19 case numbers to 251.
It appears November has been the worst month yet for coronavirus cases for the city; the start of the pandemic, from mid-March to mid-April, saw just 68 positive cases.
Luckily, there have been no new deaths reported since Sept. 1, leaving Enumclaw’s total death count at 26.
However, hospitalizations — which have been few and far between since the beginning of the pandemic — are also on the rise; seven hospitalizations have been reported since the beginning of November as of the 29th, bringing Enumclaw’s total hospitalization numbers to 35.
This rise in local hospitalizations comes amid a statewide hikes.
“COVID-19 hospital occupancy is rapidly increasing throughout Washington as the state continues to experience exponential growth in new cases,” said the Washington state Department of Health in a Nov. 25 press release. “We are seeing alarming increases in the number of COVID-19 patients in our hospitals as well as the number hospitalized in Intensive Care Unit (ICU) beds—critical capacity needed to treat severe COVID-19 cases as well as other patients with serious conditions.”
According to the DOH, roughly 72.5 percent of Washington’s total acute care beds are currently occupied (6,855 beds out of 9,453). This meets the DOH’s definition of “adequate capacity,” as less than 80 percent of all beds are taken.
Roughly 9.2 percent of the beds that are currently occupied are done so by people with COVID-19.
This may seem like a small number, but the DOH warned that it’s increasing rapidly.
“The number of confirmed and suspected COVID-19 patients in our hospitals doubled from 471 on Nov. 1 to 932 on Nov. 23,” the press release stated. “In addition, the number of confirmed and suspected COVID-19 patients in our ICUs increased about 75 percent from 124 on Nov. 1 to 214 on Nov. 23. If this doubling rate continues, we may have over 1800 COVID-19 patients in our hospitals by mid-December.”
If hospitalizations continue to increase, the DOH continued, large hospital systems may have to delay non-urgent procedures due to a lack of beds.
“Situations like this can cause other patients with non-COVID-19 conditions to have to wait, and this also impacts anyone who else may need to seek care,” the press release reads. “It is imperative that we ensure access to hospital care for anyone who needs it, whether they have COVID-19 or another illness or injury.”
It’s unclear how Enumclaw’s local hospital, St. Elizabeth Hospital, is faring with the rise in local and statewide COVID-19 cases. However, CHI Franciscan, which runs the hospital, has said it’s prepared to face the increase in case loads.
“St. Elizabeth Hospital is prepared to meet the demands and challenges presented by COVID-19. We are closely monitoring our numbers across the system to ensure we are able to manage an increasing number of COVID-19 cases, while ensuring we maintain sufficient capacity to provide the level of care needed for all patients in the hospital,” Renee Yanchura, chief operating officer at St. Elizabeth, said in a recent interview. “We monitor and work on staffing and patient placement at St. Elizabeth Hospital, and as a system.”
The health care provider added that it’s well-stocked with personal protection equipment (PPE) for its staff and patients in order to fight the rise in cases.
“Like many hospital systems, we have had to acquire significant increases in PPE than were needed prior to COVID-19, while grappling with an unpredictable national supply chain. At this time, CHI Franciscan is currently well-sourced with Simple and N95 masks, eyewear and higher level PPE needed in specific situations,” Yanchura said, without specifying how many days or weeks of PPE the system has on hand. “We approach PPE sourcing not just as a single hospital or region, but as an entire system. We can rely on our national resources to help track down additional PPE if we are in need locally.”
Despite the rise in cases, Yanchura stressed that people facing a medical emergency to not delay care.
“St. Elizabeth Hospital has been, and is continuing to take, a number of steps to make sure that our hospitals and emergency services departments are implementing the top safety measures possible,” she added. “The sooner you seek treatment for emergencies like heart attacks, strokes, or traumatic injuries, the better care we are able to provide.”